Overview
Traumatic brain injury (TBI), or concussion is a common cause of death in the United States. This condition is often difficult to manage because patients present a range of subtle symptoms that may appear suddenly. There are number of ways patients and doctors can help , one of the ways is to use brian injury medicine or medication, I will discuss it in the following paragraphs.
According to the Centers for Disease Control and Prevention (CDC), experts noticed a 53% rise in the number of TBI-related emergency department visits, hospital admissions, and fatalities from 2006 to 2014.
What’s more, living through a concussion doesn’t always mean you will return to normal life. You see, survivors may spend the remainder of their lives dealing with severe neurological symptoms, making this a truly daunting condition to manage.
In this article, we will cover the causes and symptoms of traumatic brain injury, as well as how we can diagnose it. After that, we will discuss some medications for traumatic brain injury.
How does a brain injury occur
To fully understand how you can suffer a concussion, it’s crucial to grasp the structure of a neuron or brain cell. Each neuron consists of a cell body, dendrites, and an axon. The human brain contains billions of these neurons, which communicate via dendrites and axons.
The brain resembles gelatin in texture and consistency. While the skull provides a protective shield against external blows, it can sometimes be a double-edged sword. Picture your brain moving within your skull, with no barrier separating it from the hard, bony structure. This scenario could be quite debilitating.
Whenever we shake our heads, stand up, or sprint, our brains could make powerful contact with the skull, leading to possible damage. To prevent this, we have the cerebrospinal fluid (CSF) encircling the brain, functioning as a shock absorber to reduce the friction between the brain and the skull. In summary, your brain floats in the CSF to facilitate easy movement when you change positions.
After covering the anatomy of the brain, let’s delve into concussions.
A concussion results when the brain hits the skull with a force that exceeds the CSF’s cushioning capacity. The brain briefly compresses, sending shock waves throughout, which rip apart the axons of some neurons. This event is known as a diffuse axonal injury.
The tearing of axons disrupts the intraneuronal network, resulting in reduced brain functionality.
The different types of traumatic brain injury
Traumatic Brain Injuries (TBIs) can be broadly categorized based on their severity, with factors such as loss of consciousness duration, neurological symptoms onset, memory loss surrounding the event, and abnormalities in head CT or brain MRI playing a role in this classification.
- Mild Concussion (mTBI) – This type accounts for three-quarters of all TBIs annually. An mTBI may involve a transient loss of consciousness, presenting as feeling dazed or unconscious lasting less than 30 minutes. Following an mTBI, confusion may persist for a day.
- Moderate TBI – This injury level corresponds with a loss of consciousness spanning over 30 minutes but less than a day. Confusion may extend up to a week in moderate TBI.
- Severe TBI – These injuries involve a loss of consciousness exceeding a day. Often, severe TBIs are linked to visible changes on head CT or brain MRI.
The complexity of the injury further subdivides TBIs into:
- Uncomplicated TBI – Irrespective of the severity grading (mild, moderate, or severe), the head CT/brain MRI appears normal.
- Complicated TBI – In contrast to uncomplicated TBIs, these show changes on head CT or brain MRI, such as bleeding.
- Closed TBI – This form of TBI is the most common, occurring when an external force blows the head without breaching the skull, causing brain injury and swelling.
- Open TBI – Also known as a penetrating TBI, these injuries occur when an object, such as a bullet or knife, penetrates the skull, causing direct damage to the brain tissue.
- Nontraumatic TBI – Not all TBIs result from trauma. Strokes, seizures, near-drowning incidents, and choking can also lead to TBIs. We refer to this type of TBI as hypoxic/anoxic brain injuries.
Signs and symptoms of traumatic brain injury
Symptoms of a concussion can vary dramatically based on which part of the brain is impacted. For instance, a traumatized frontal lobe might lead to confusion, headaches, and impaired muscular coordination.
Other common symptoms include:
- Headaches
- Nausea
- Vomiting
- Dizziness
- Sensitivity to light
- Blurred vision
- Ringing in the ears
- Slurred speech
- Loss of consciousness
- Memory loss
- Irritability
- Depression
These symptoms are shared with other neurological conditions, making it quite difficult to tell concussions apart. This is especially problematic when healthcare professionals cannot get a medical history of the patient.
How to diagnose a traumatic brain injury
To diagnose concussions, your doctor will:
- Collect your medical history
- Conduct a comprehensive physical examination
- Order a few imaging tests
Medical practitioners will start by asking questions to collect a history of physical trauma and potential risk factors. After that, your doctor will conduct a neurological examination to detect signs consistent with a concussion diagnosis. If severe symptoms are present, he/she may order an MRI or CT scan to visualize the brain and pinpoint the damaged area.
Once a concussion is confirmed, the focus shifts to medical or surgical treatment.
The treatments for brain injury
Individuals who suffer from mild to moderate TBIs might only require some basic care, such as taking a pause from athletic activities, school, and work. Usually, symptoms should start to subside within several weeks.
However, for severe TBIs, patients frequently need hospitalization and more rigorous treatment procedures, such as brain injury medicine.
Regardless of the severity of TBI, treatment options might encompass:
- Counseling for Emotional Support – Those suffering from TBIs often encounter stress and anxiety concerning their recovery journey. The challenge of resuming work and hobbies can be quite challenging. Therefore, psychological counseling frequently might be beneficial in conjunction with other medical interventions.
- Surgery – Surgical intervention may be necessary to address bleeding, which is known as intracranial hemorrhage.
- Rehabilitation – Rehabilitative measures might involve physical therapy, occupational therapy, and speech therapy.
Natural concussion remedy
While taking brain medicine injury or surgery might be necessary, some natural remedies can also support the healing process.
For example, adequate hydration is indispensable for recovery, aiding the body’s natural healing mechanisms. Moreover, omega-3 fatty acids, which are found in foods like fish, chia seeds, and walnuts, can support brain health and potentially expedite recovery.
Antioxidant-rich foods, including fruits and vegetables, can also help minimize inflammation and oxidative stress. Furthermore, light physical activity (e.g., walking) can promote blood flow to the brain.

While mindfulness practices, such as meditation and yoga, can aid in reducing stress and promoting mental well-being. Nonetheless, opting for a natural concussion remedy should supplement and not replace professional medical treatment. It’s crucial to consult with a healthcare provider to guide the concussion recovery process and suggest where to buy brain injury medicine.
It’s crucial to consult with a healthcare professional regarding the appropriate rest duration following a TBI. Depending on the severity of the injury, some individuals might need to rest for a day or two before resuming normal activities. However, more serious injuries could necessitate extended rest periods.
For individuals with mild injuries, prolonged rest periods post-injury might create difficulties in returning to work, school, and recreational activities. On the other hand, resuming activities prematurely following more severe injuries can exacerbate symptoms. Therefore, it is essential to obtain specific advice from a medical professional regarding a safe and effective return to daily activities.
Medications for traumatic brain injury
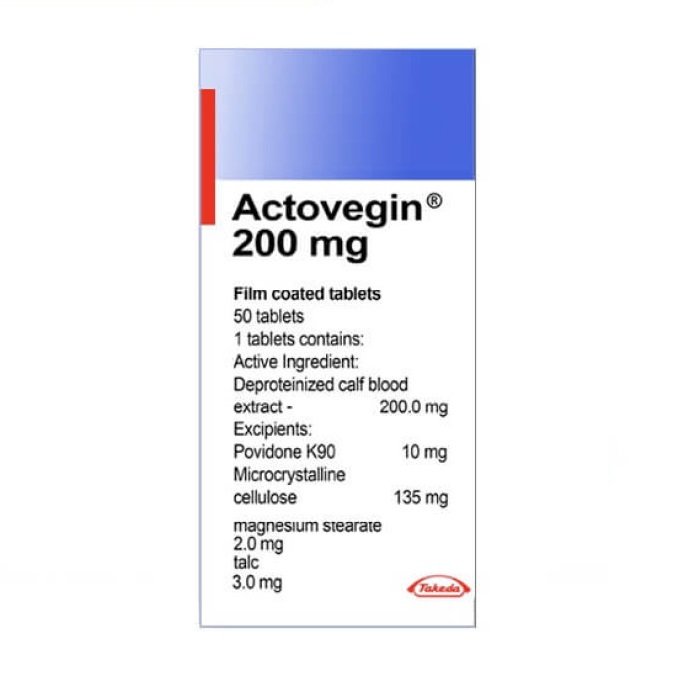
Actovegin is a highly purified extract derived from calf blood. This drug contains bioactive ingredients, such as inositol phospho-oligosaccharides (IPOs), which can cross the blood-brain barrier due to their small size.
There is also some evidence that Actovegin might be the best medicine for brain injury. Researchers found that this medicine possesses neuroprotective and neuroregenerative properties.

It also supports tissue survival in lesions, reduces the degeneration of peripheral neurons, and improves their functionality. These benefits may be attributed to its anti-oxidative and anti-apoptotic properties thanks to anti-poly (ADP-ribose) polymerase (PARP) activation.
In a study conducted at the Bagdasar-Arseni Teaching Emergency Hospital in Bucharest, scientists compared the outcomes of patients treated with Actovegin after a concussion to those receiving standard therapy. Researchers administered Actovegin as two 200mg tablets per day. Consequently, patients showed significantly higher scores for:
- Functional Independence Measure (FIM)
- Disability Rating Scale (DRS)
- Glasgow Outcome Score (GOS)
- Modified Rankin (Disability) Score (mR(D)S)
- Activities of Daily Living (ADL)
These results suggest that Actovegin does improve functional outcomes following a TBI, making it the best medicine for head injury.
You way ask , is Actovegin a safe brain injury medicine. The answer is actovegin has been in use for almost 55 years in various neurologic conditions, including TBIs, ischemic and hemorrhagic strokes, age-related cognitive impairments, dementia-related behavioral conditions, and diabetes mellitus including secondary polyneuropathy. Additionally, it has been found safe for use in patients with concurrent conditions, such as epilepsy and diabetes mellitus, commonly encountered in neurorehabilitation practice. This shows how safe Actovegin has been for 6 decades as brain injury medication.
Further reading
Daia, C., Scheau, C., Spinu, A., Andone, I., Popescu, C., Toader, C., Bumbea, A. M., Verenca, M. C., & Onose, G. (2021). Modulated Neuroprotection in Unresponsive Wakefulness Syndrome after Severe Traumatic Brain Injury. Brain sciences, 11(8), 1044. https://doi.org/10.3390/brainsci11081044
Reichl, F. X., Högg, C., Liu, F., Schwarz, M., Teupser, D., Hickel, R., Bloch, W., Schweikl, H., Thomas, P., & Summer, B. (2020). Actovegin® reduces PMA-induced inflammation on human cells. European journal of applied physiology, 120(7), 1671–1680. https://doi.org/10.1007/s00421-020-04398-2
Ziegler, D., Movsesyan, L., Mankovsky, B., Gurieva, I., Abylaiuly, Z., & Strokov, I. (2009). Treatment of symptomatic polyneuropathy with actovegin in type 2 diabetic patients. Diabetes care, 32(8), 1479–1484. https://doi.org/10.2337/dc09-0545
Meilin, S., Machicao, F., & Elmlinger, M. (2014). Treatment with Actovegin improves spatial learning and memory in rats following transient forebrain ischaemia. Journal of cellular and molecular medicine, 18(8), 1623–1630. https://doi.org/10.1111/jcmm.12297
Machicao, F., Muresanu, D. F., Hundsberger, H., Pflüger, M., & Guekht, A. (2012). Pleiotropic neuroprotective and metabolic effects of Actovegin’s mode of action. Journal of the neurological sciences, 322(1-2), 222–227. https://doi.org/10.1016/j.jns.2012.07.069
Firan, F. C., Romila, A., & Onose, G. (2020). Current Synthesis and Systematic Review of Main Effects of Calf Blood Deproteinized Medicine (Actovegin®) in Ischemic Stroke. International journal of molecular sciences, 21(9), 3181. https://doi.org/10.3390/ijms21093181